

Affiliations
ABSTRACT
Brucellosis is a common zoonotic disease in the world and in Turkiye. The disease is transmitted to humans through ingestion of unpasteurized animal milk products or direct contact with infected tissues or fluids. Brucellosis typically presents with nonspecific symptoms such as intermittent fever, night sweats, myalgia, and arthralgia, but may present along with numerous other clinical signs and complications. Herein, we report a case of acute cholecystitis, a rare complication of brucellosis, presenting with fever, abdominal pain, and elevated liver enzymes.
Key Words: Acute cholecystitis, Brucellosis, Zoonoses.
INTRODUCTION
Acute cholecystitis is a clinical condition characterised by the inflammation of the gallbladder. Gallstones are the cause in 95% of the cases, but acute acalculous cholecystitis is known to occur in 5% of the cases.¹ Typical symptoms of acute cholecystitis include fever, nausea, and right upper quadrant pain. Brucellosis is a zoonotic disease transmitted from infected animals to humans through ingestion of unpasteurized animal milk products or direct contact with infected tissues or fluids and inhalation of infected aerosolized particles. The disease is characterised by non-specific symptoms such as intermittent fever, malaise, night sweats, and arthralgia. Although liver involvement is classical in brucellosis, acute cholecystitis is rare. Herein, a brucellosis-associated cholecystitis case is presented.
CASE REPORT
A 30-year-old male presented to the outpatient clinic with a complaint of abdominal pain. His temperature on admission was 38.8°C; blood pressure, 120/70 mmHg; heart rate, 120 bpm, and oxygen saturation, 98%. There was tenderness in the right upper abdominal quadrant and a positive Murphy sign. Hepatobiliary ultrasonography (US) reported hepatomegaly and thickening of the gallbladder wall, with an increase in density in favour of oedema/inflammation in the pericholecystic fat, compatible with acute cholecystitis.
Abdominal computed tomography (CT) was also compatible with cholecystitis (Figures 1 and 2). The patient was hospitalised in the general surgery unit. An antibiotic therapy with ceftriaxone 1 g intravenously twice a day (bid) and metronidazole 500 mg thrice a day was started. Three days after the start of the antibiotic therapy, the fever persisted. The laboratory tests showed white blood cells (WBC) count of 2090/ul; neutrophils, 1360/ul; platelets (PLTs), 140000 /L; C-reactive protein (CRP), 42 mg/dl; alanine transaminase (ALT) 303 U/l, aspartate transaminase (AST) 303 U/l, alkaline phosphatase (ALP) 222 U/l, gamma-glutamyltransferase (GGT) 128 U/l; total bilirubin 1.5 mg/dl; direct bilirubin 0.6 mg/dl; and creatinine 0.66 mg/dl. The patient reported a history of eating unpasteurized food products. Brucella rose bengal test was positive and the tube agglutination test with Coombs was found to be 1/640. Ceftriaxone and metronidazole treatments were stopped. Blood cultures were performed. Doxycycline 100 mg bid and rifampicin 600 mg daily were started. Fever regressed within 72 hours after antibiotic treatment onset. Blood cultures were positive for Brucella spp. growth. The elevated liver enzymes regressed (Table I) and the patient was discharged on 10th day of hospitalization on doxycycline and rifampicin. His complaints completely regressed and treatment was completed in 8 weeks.
DISCUSSION
Brucellosis is a zoonotic disease that is endemic in Turkiye as in many parts of the world. Worldwide, 500000 new cases of brucellosis occur every year.² According to the data of the Turkish Ministry of Health, the morbidity rate of the disease in this country is 7.9/100000.³ The disease typically presents with nonspecific symptoms such as intermittent fever, night sweats, malaise and arthralgia. However, since it is a multisystem disease, it may mimic many diseases in its clinical and laboratory findings.
Table I: Laboratory findings during the patient's hospital course.
|
|
AST (U/L) |
ALT (U/L) |
ALP (U/L) |
GGT (U/L) |
WBC(/L) |
PLT (/L) |
CRP (mg/dL) |
|
1st day |
303 |
303 |
222 |
128 |
2090 |
140 000 |
42 |
|
3rd day |
979 |
712 |
230 |
124 |
2710 |
126 000 |
35 |
|
5th day |
643 |
212 |
200 |
116 |
3700 |
178 000 |
8 |
|
7th day |
500 |
157 |
181 |
109 |
5900 |
217 000 |
2 |
|
10th day |
274 |
91 |
158 |
96 |
6810 |
268 000 |
1 |
|
AST: Aspartate transaminase, ALT: Alanine transaminase, ALP: Alkaline phosphatase, GGT: Gamma glutamyltransferase, WBC: White blood cells, PLT; Platelet, CRP: C-reactive protein. |
|||||||
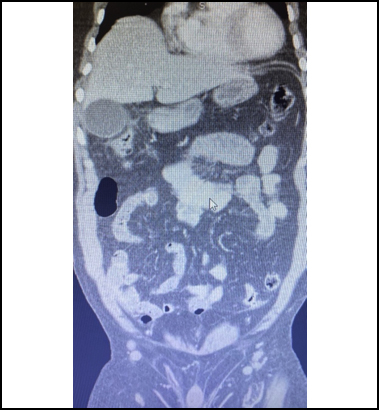 Figure 1: Abdominal CT scan (coronal section) showing the increase in thickness of gall bladder wall and oedema.
Figure 1: Abdominal CT scan (coronal section) showing the increase in thickness of gall bladder wall and oedema.
Focal brucellosis is seen in approximately 30% of cases.⁴ The most common complication is osteoarticular system complication such as arthritis, spondylodiscitis and sacroiliitis. The most common gastrointestinal complication of brucellosis is hepatitis. Intra-abdominal manifestations such as liver or splenic abscess, cholecystitis, pancreatitis, ileitis, colitis and peritonitis are rare focal organ complications of brucellosis.5
Approximately 30 cases of cholecystitis associated with brucellosis have been reported in the literature. Of these, 4 were reported after 2019.6-8 All patients had clinical symptoms of acute cholecystitis and a history of fever starting days before presentation. B. melitensis was grown in the blood cultures of 12 patients and in the intraoperative bile cultures of eight patients, and B. melitensis was grown in both blood and bile cultures in five patients.
B. abortus was isolated in bile culture in one patient and B. suis was isolated in both blood and bile cultures in one patient. Three patients who had no Brucella spp. growth in blood and bile cultures who were also negative for Brucella polymerase chain reaction (PCR), were diagnosed with positive serological tests.
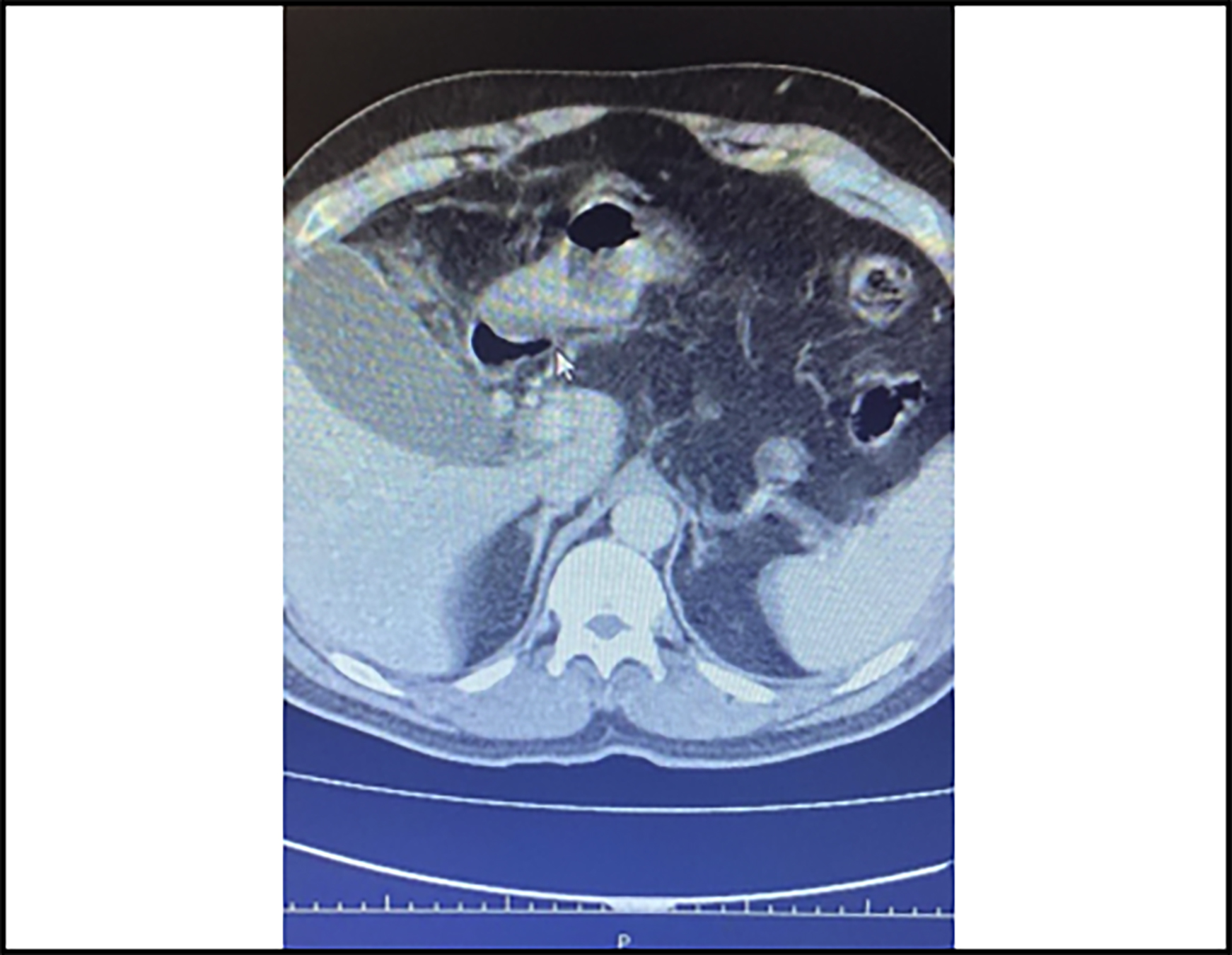 Figure 2: Abdominal CT scan (axial section) showing the increase in thickness of gall bladder wall and oedema.
Figure 2: Abdominal CT scan (axial section) showing the increase in thickness of gall bladder wall and oedema.
In this case, abdominal pain, fever and night sweats were present as in other cases. B. melitensis was grown in both blood cultures of the patient who had a long history of high fever and a history of eating unpasteurised food products. No response was obtained from ceftriaxone treatment initiated on a diagnosis of cholecystitis, but a favourable response was obtained on the 3rd day of doxycycline and rifampicin treatment.
Culture is the gold standard for diagnosis in brucellosis. Pre-diagnosis is made by detecting Brucella deoxyribonucleic acid (DNA) in the serum sample by PCR test or a Brucella spp. total antibody titre above 1:160 can be used by standard tube agglutination test.⁹
First-line treatment consists of antibiotics with intracellular activity such as tetracyclines, aminoglycosides and rifampicin. Fluoroquinolones and trimethoprim-sulfamethoxazole are alternative treatment options.¹⁰ Combination therapy (doxycycline and rifampicin/gentamicin/streptomycin) is recommended for at least 6 weeks. The optimal duration of treatment for intra-abdominal complications of brucellosis has not been determined.⁸ Combination of gentamicin/streptomycin or rifampicin with doxycyline for duration of 6-12 weeks is the most commonly used therapeutic approach. In this case, as in most cases in the literature, doxycycline 100 mg bid and rifampicin 600 mg daily oral were used for 6 weeks. No recurrence was observed during the three-month follow-up period.
In conclusion, this case is important in terms of contributing to the literature because it presents a rare complication of a relatively common disease. Although gallstones are the most common cause of acute cholecystitis, this complication of brucellosis should be kept in mind, especially in people living in endemic areas and with a history of occupational exposure.
PATIENT’S CONSENT:
Informed consent was obtained from the patient.
COMPETING INTEREST:
The author declared no competing interest.
AUTHOR’S CONTRIBUTION:
YC: The conception or design of the work, the acquisition, analysis or interpretation of data for the work, drafting the work or revising it critically for important intellectual content. Final approval of the version to be published.
REFERENCES
Copyright © 2025. The author(s); published by College of Physicians and Surgeons Pakistan. This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY-NC-ND) 4.0 https://creativecommons.org/licenses/by-nc-nd/4.0/ which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.