

Affiliations
ABSTRACT
Papillary thyroid microcarcinomas (PTMCs) are subcentimetre papillary carcinomas with benign behaviour. Infiltrative follicular subtype of PTMC (IFPTMC) is considered an indolent lesion with propensity to nodal metastasis. Here, we report a case of unifocal IFPTMC with no lymphadenopathy, presenting with fracture of humerus due to metastasis.
A 57-year female patient presented with right humerus pathological fracture. MRI of the right humerus revealed a neoplastic deposit. Bone and soft tissue biopsy showed neoplastic cells resembling thyroid carcinoma. The whole body I-131 scan exhibited increased uptake in the right humerus lesion. Total thyroidectomy was performed. The histopathological report of the specimen showed IFPTMC.
Treating PTMC aggressively with total thyroidectomy has, no doubt, led to a worldwide epidemic of thyroid cancers. But are we confident enough to render active surveillance as their only treatment? Research work is still needed to identify the prognostic factors of PTMC that could guide clinicians to choose appropriate treatment.
Key Words: Thyroid, Papillary microcarcinoma, Follicular subtype, Bony metastasis.
INTRODUCTION
According to World Health Organisation’s histologic classification Papillary Thyroid Micro carcinoma (PTMC) is defined as sub centimetre lesion having the largest dimension ≤10 mm.
It has been stated that over-diagnosis and over-treatment of PTMC are leading to the worldwide epidemic of thyroid carcinoma.1 Thus, its incidence has increased from 30% in 1988 to 40% in 2003.2
Being indolent in its course with an excellent prognosis, the clinical significance of PTMC is still questionable. Its cancer-related mortality rate is just 0.34%.3 Its standard treatment is highly controversial, the recommendations ranging from total thyroidectomy to active surveillance.1 Clinically impalpable, most of the PTMCs are found incidentally during histopathological examinations of thyroid specimens obtained during autopsy/surgery for non-malignant thyroid diseases. Up to 18% of patients have palpable adenopathy at the time of presentation,2 while distant metastasis as first presentation is very rare, almost 0.37%.3
Here, we present a case of PTMC, in which the initial and the only presentation was pathological fracture of humerus due to metastasis.
CASE REPORT
A 57-year female, with no previous comorbidities, presented with pain, swelling, and non-traumatic deformity of the right upper arm. Her family, past medical, and past surgical histories were unremarkable.
General physical examinations showed vitally stable patient, having 61 kg weight, 150 cm height, and a body mass index (BMI) of 27.1.
Local examination revealed tenderness with swelling of the right mid-arm and mild internal rotation of the forearm. The overlying skin was intact. Brachial, radial, and ulnar pulses were palpable. The rest of the neurovascular examinations were unremarkable.
X-ray of the right humerus showed a midshaft comminuted fracture. Contrast-enhanced MRI of the right arm showed a poorly marginated linear area of abnormal MR signal in the midshaft of the right humerus (56 × 15 mm) suggesting myeloma or metastatic deposit. Contrast-enhanced CT scan of the chest, abdomen, and pelvis was unremarkable.
Right humerus fracture reduction with intramedullary implant was done by the orthopaedic team and soft tissue and bone fragments were obtained for histopathology which revealed morphological features of the neoplastic lesion, exhibiting tubule formation and diffuse arrangement. Individual cells had eosinophilic cytoplasm with oval hyperchromatic nuclei.
Table I: Comparison of clinicopathological features of T1a N0 M1 cases of papillary thyroid microcarcinoma.
|
Author / Year |
Age (years)/ Sex |
Site of Metastasis |
Histo- |
Tumour size (mm) |
BL |
MF |
CI |
VI |
ETE |
|
Lin8 |
75/F |
Skull |
NA |
10 mm |
NA |
NA |
NA |
NA |
NA |
|
Erdem9 |
40/M |
Parapharyngeal |
NA |
8 mm |
NA |
NA |
NA |
NA |
NA |
|
Lecumberri9 |
65/F |
Cerebellum |
Diffuse Sclerosing |
2 mm |
NA |
NA |
+ |
+ |
NA |
|
Saito9 |
70/F |
Lung |
NA |
8 mm |
NA |
NA |
NA |
NA |
NA |
|
Shawky8 |
59/M |
Brain (Frontal lobe) |
Classic |
3 mm |
+ |
+ |
- |
- |
- |
|
Yang10 |
26/F |
Liver, Lung |
Classic, |
NA |
- |
+ |
+ |
NA |
NA |
|
Present case |
57/F |
Bone |
Infiltrative Follicular |
5 mm |
- |
- |
- |
- |
Microscopic |
|
BL, Bilaterality; CI, Capsular Invasion; ETE, Extrathyroidal Extension; F, Female; M, Male; MF, Multifocality; NA, Not Available; VI, Vascular Invasion |
|||||||||
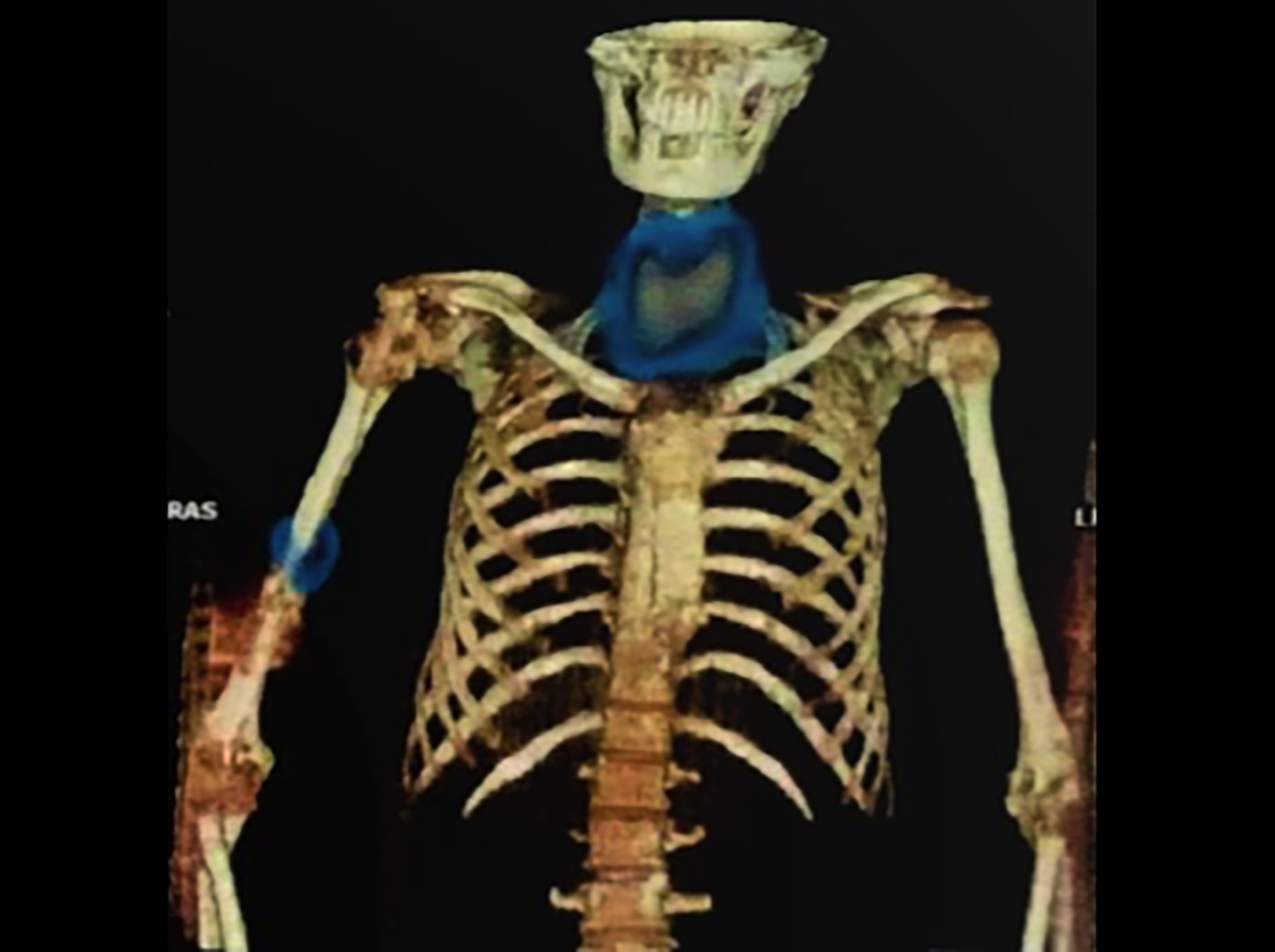 Figure 1: Whole body I-131 scan with complementary SPECT showing normal tracer uptake in thyroid with focal area of increased uptake in right humerus at the site of pathological fracture.
Figure 1: Whole body I-131 scan with complementary SPECT showing normal tracer uptake in thyroid with focal area of increased uptake in right humerus at the site of pathological fracture.
Immunohistochemical studies of the specimen showed positive reactivity for TTF-1, PAX-8, Cytokeratin-7, and Thyroglobulin (TTG), pointing at the thyroid gland as the primary site of tumour. Ultrasonography of the neck was unremarkable.
Significant haematological studies included increased Thyroglobulin levels (128 ng/ml), Alkaline Phosphatase (434 u/L), and raised uric acid (6.2 mg/dL). Whole body I-131 scan with complementary SPECT revealed normal tracer uptake in the thyroid with increased uptake in the right humerus at the site of pathological fracture (Figure 1).
Under general anaesthesia, total thyroidectomy with neck dissection was performed. Per operatively, except for fibrosis around the right lobe, the rest of the thyroid gland and surrounding tissues were grossly unremarkable.
In histopathological examinations, grossly, the specimen revealed a 5×3 mm greyish-white suspicious area on the cut surface of the right lobe of the thyroid. The histological examination showed IFPTMC, with microscopic extrathyroidal extension (ETE). Neither a tumour capsule nor lymphovascular invasion could be identified. The tumour was staged as T1a, N0, M1.
Currently, the patient is under radioiodine ablation therapy.
DISCUSSION
In the 2022 WHO Classification of Thyroid Tumors, 5th edition, PTMC is no longer considered as a separate subtype of papillary thyroid carcinoma (PTC). Instead, it has been stated that such lesions must undergo histologic subtyping and be classified under the distinct subtypes of PTC.4
Infiltrative follicular subtype of PTC (IFPTC) constitutes almost 17% of PTMC.2 IFPTC has behavior and molecular profile very close to that of classical PTC, showing a propensity to nodal metastasis and local invasive growth.4 It has been regarded as an indolent and benign subtype of PTC as compared to other aggressive subtypes like tall cell, columnar cell, and hobnail PTCs.2
Distant metastatic potential of PTMC has been reported as 0.1%.5 But literature is still lacking in reporting the distant metastatic potential of IFPTMC. While working on prognostic features of PTMC, Jeon et al. reported cervical nodal metastasis with extra-nodal extension or aggressive subtypes to be significantly associated with distant metastasis.5 On the contrary, this patient neither had any cervical lymphadenopathy nor aggressive histologic subtypes. A similar study done by Mercante et al. regarded macroscopic ETE, capsular invasion and lymph node metastasis as the risk factors for distant metastasis.6 In the present case, the capsular invasion was not applicable, while there was only microscopic ETE with no nodal metastasis. Some studies are in favour of multifocality as a predictor of worst outcomes in PTMC.2 In the present patient, the lesion was unifocal. However, Huang et al. reporting the patient’s age either ≤30 or >45 years at the time of diagnosis, as a risk factor for distant metastasis, is supported by the present case being 57 years old.7
Among all the prognostic factors, lymph node metastasis at presentation has been regarded as the most frequent adverse feature for distant metastasis.5,6,8,9 However, we searched the literature, available in the English language, for the PTMC with distant but no nodal metastasis. All those cases were excluded in which data regarding nodal metastasis was missing (Table I).
In Table I, none of the clinicopathological factors were consistent among reported T1aN0M1 cases. Reviewing the results of studies done in various countries, Vaccarella et al. suggested that watchful waiting should be considered a preferable option in patients with low-risk PTMC, in order to avoid overdiagnosis and overtreatment.1 The present case with low-risk PTMC, neither having any local disease, nor having any bad prognostic feature, presented with distant metastatic crisis, and needed an aggressive therapeutic approach.
Treating PTMC aggressively with total thyroidectomy with or without radioactive iodine ablation therapy, the so-called overtreatment, has, no doubt, led to a worldwide epidemic of thyroid cancers. But are we confident enough to render active surveillance as their only treatment? Further research work is needed to identify the prognostic factors of PTMC that could guide clinicians to choose appropriate treatment.
PATIENT’S CONSENT:
The authors, hereby, certify that appropriate informed written consent was obtained from the patient and her attendant regarding the use of her clinical information, both descriptive and photographic, for academic and publication purposes. The patient understands that her identity will be concealed during the process but the authors cannot guarantee her anonymity.
COMPETING INTEREST:
The authors declared no competing interest.
AUTHORS’ CONTRIBUTION:
NL: Conception and drafting of the manuscript.
SS: Conception and data collection.
IU: Data interpretation.
IUH: Data collection and drafting of the manuscript.
SU: Drafting.
All authors have approved the final version of the manuscript to be published.
REFERENCES
Copyright © 2025. The author(s); published by College of Physicians and Surgeons Pakistan. This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY-NC-ND) 4.0 https://creativecommons.org/licenses/by-nc-nd/4.0/ which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.