

Affiliations
ABSTRACT
Differentiating between benign cutaneous manifestations and lesions from inflicted injuries is not always simple. A 14-year boy was admitted to our Forensic Medicine Clinic for the preparation of a medico-legal report requested by the prosecution office. On inspection, there were 10 violaceous, atrophic, horizontal, linear striae distensae (SD), confined to the lower back and measuring 0.5 cm in width and between 6 cm and 13 cm in length. The boy had experienced severe weight loss and a large spurt in height in recent months. A diagnosis of physiologic SD was made. This case is presented to draw physicians’ attention to a physiologic skin manifestation in adolescence that mimics trauma. It is recommended that practitioners develop examination skills and medical knowledge about cases that may become the subject of legal action. Moreover, physicians should learn to distinguish whether skin lesions originate from trauma or not.
Key Words: Stretch marks, Physiologic striae, Physical child abuse, Forensic medicine.
INTRODUCTION
Striae distensae (SD) are cutaneous lesions also known in the literature as atrophic striae, the physiologic striae of adolescence, striae gravidarum, or stretch marks.1,2 SDs were first identified in the literature of medicine in 1829.3
Not only do SDs occur as scar tissue in the dermis layer, but also atrophy emerges in the epidermis layer.3 SDs appear as a skin streak that can turn out to be a result of Cushing syndrome, female gender, treatment with steroids or antibiotics, infection, pregnancy, obesity, or adolescence.1,3 The pathogenesis of SDs is still unknown, but it is most commonly thought to depend on the alteration of the extracellular matrix constituents that balance cutaneous elasticity and resistance to stretching.1
A physician may be presented with a suspicious cutaneous manifestation derived from trauma and should learn to discriminate between common skin signs of normal and inflicted injury. These cutaneous manifestations are frequently seen in adolescents and may be diagnosed incorrectly as physical abuse.2 The aim of this presentation is to describe a rare case in which benign cutaneous lesions were mistakenly diagnosed as injury-related wounds.
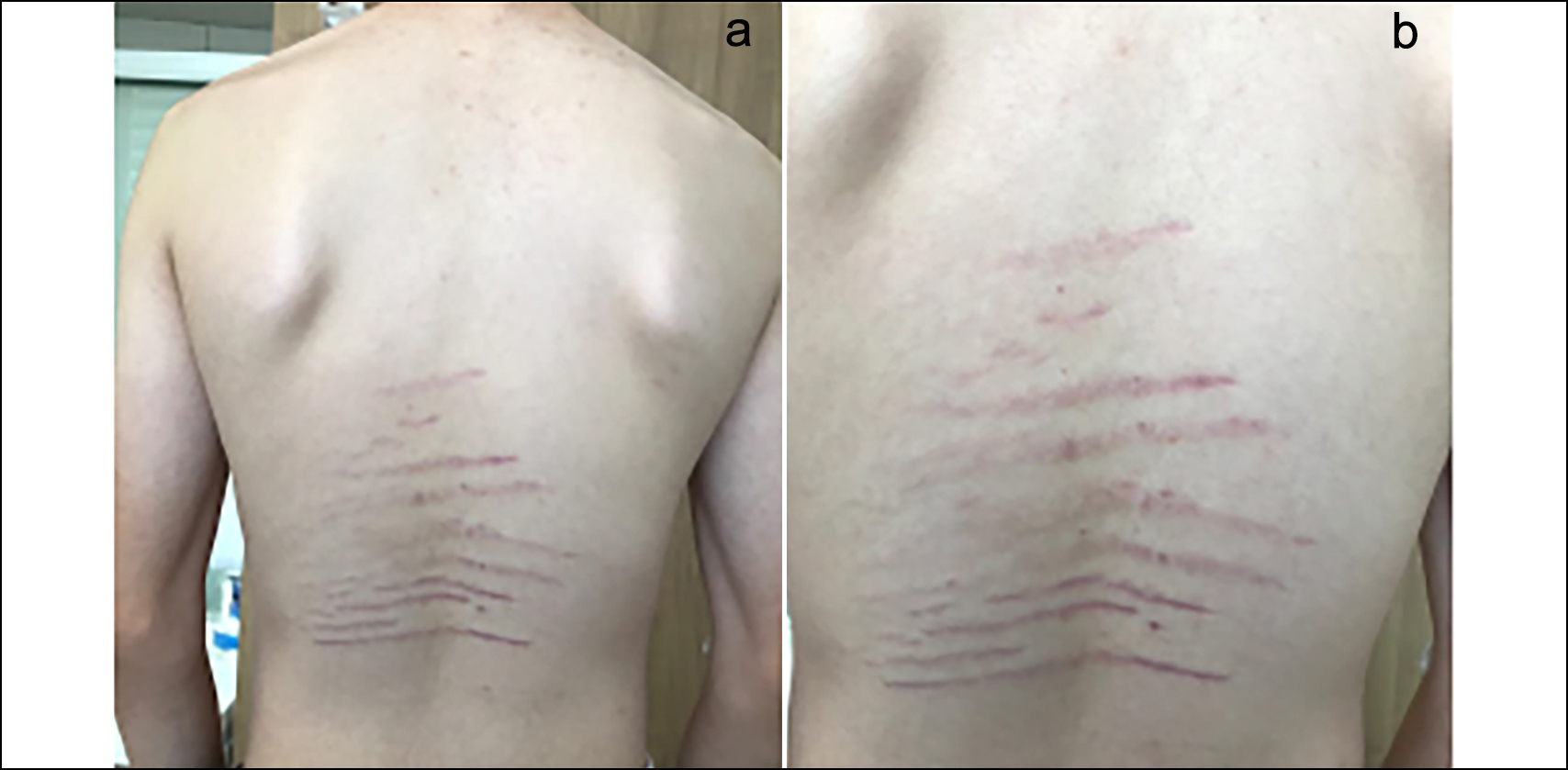 Figure 1 (a, b): Striae distensae confined to the lower back.
Figure 1 (a, b): Striae distensae confined to the lower back.
CASE REPORT
A 14-year boy was admitted to the Emergency Department (ED) of the Kastamonu State Hospital in Turkey with common cold symptoms. While auscultation was being performed, the practitioner discovered many suspicious skin markings on the back of the patient, and diagnosed physical child abuse, whereupon he referred the case to the legal authorities. Three days later, the patient was admitted to our Forensic Medicine Clinic for the preparation of a medico–legal report requested by the prosecution office. He weighed 59 Kg and was 185 cm tall. He reported that he had grown in height by 5 cm and lost 5 kg in weight only in the previous three months. He had not been involved in any sporting activity nor had a surgical intervention. Moreover, there was no history of accident or injury or any disease, including joint problems or connective tissue disorders. He said that he had not used any medications in the recent past.
Dermatological examination revealed 10 violaceous, atrophic, horizontal, linear SD on the lower back, measuring approximately 0.5 cm in width and between 6 cm and 13 cm in length (Figure 1a, b). The patient had experienced severe weight loss and a rapid growth in height in recent months. A diagnosis of physiologic SD was made and confirmed by a consultant dermatologist.
DISCUSSION
In the present case, SD occurred only on the lower back, and there was no obvious cause. In recent cases, three teenagers presented with SD on the back and gluteal region.2,4,5 One of these was a 14-year boy with back pain and SD in the lumbosacral region. The examiner mistakenly described these lesions as physical abuse and referred the boy to social services.2 Another case was that of a 16-year boy whose mother alleged that the markings were caused by physical assaults by his schoolmates during episodes of bullying. However, upon examination, a diagnosis of SD was made.6
In the literature, other SD cases without any obvious cause are widely reported. One such was a 16-year boy with SD on his unilateral axilla.7 Another was a 14-year boy with SD on the lower back, who also suffered from coeliac disease.8 An 18-year girl suffered from SD on her legs, accompanied by ileitis.3 A further case was that of a 14-year boy with SD on both lateral thighs.9
Previous studies found approximately the same age onset for the SDs. A study found the median age to be 14.3 years.10 Similarly, the patient in the present case had a rapid growth spurt, reaching a tall stature.10 One study that investigated 12 boys with SDs on the lower back revealed that SDs were seen most frequently in normal or tall adolescents of low weight.10 In contrast to the present case, the increase in weight was purported to give rise to the development of longitudinal SD.3
Accurate and early diagnosis of these benign cutaneous manifestations is important for physicians to avoid being wrongly accused of incorrect diagnoses. It is vital for paediatricians, emergency medicine specialists, general practice specialists, and especially forensic medicine specialists to be familiar with this situation. It is recommended that physicians consider phenomena that mimic physical child abuse, develop their examination skills and knowledge of this subject, and adopt a multidisciplinary approach to complicated cases to ensure early and accurate diagnosis.
PATIENT’S CONSENT:
The patient and his relatives provided written informed consent for this unusual case to be reported in a medical journal.
COMPETING INTEREST:
The authors declared no competing interest.
AUTHORS’ CONTRIBUTION:
SK, MY: Substantial contributions to the conception or design of the work, acquisition, analysis, and interpretation of data.
SK, MY, RF: Drafting the manuscript and revising it critically for important intellectual content.
All the authors have approved the final version of the manuscript to be published.
REFERENCES
Copyright © 2025. The author(s); published by College of Physicians and Surgeons Pakistan. This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY-NC-ND) 4.0 https://creativecommons.org/licenses/by-nc-nd/4.0/ which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.