

Affiliations
ABSTRACT
A young patient presented to the emergency room (ER) with Type B aortic dissection and ascending aorta aneurysm. He was planned for medical optimization, close surveillance, echocardiography, and ascending aorta replacement on an urgent basis. His surveillance echocardiogram 2 days later revealed that Type B aortic dissection has converted into Type A aortic dissection. Therefore, “Emergency Type A aortic dissection repair with Aortic root and ascending aorta replacement” was planned. The pericardial cavity was full of blood as the aneurysm had ruptured. Partial circulatory arrest along with an antegrade cerebral perfusion was maintained for distal anastomosis. A 25-sized SJ aortic valve- conduit was used for root replacement. The patient did very well and got discharged from the hospital on the sixth postoperative day.
Key Words: Type A aortic dissection, Aortic root and ascending aorta aneurysm, Type B aortic dissection.
INTRODUCTION
The prime line of treatment for an uncomplicated Type B aortic dissection (TBAD) is medical therapy.1 With new advancements, thoracic endovascular aortic repair (TEVAR) is now considered the favoured option for uncomplicated TBAD.2 On the other hand, type A aortic dissection is regarded as a surgical emergency with a mortality rate of 0.5% per hour without surgery. It reduces to 0.09% per hour in those receiving surgery.3 Ascending aortic aneurysm (AAA) is a surgical urgency when size increases by more than 5.5 cm.4 This is a rare case report of a young patient who presented with the diagnosis of TBAD and AAA of 6.6 cm which converted into Type A aortic dissection and became a surgical emergency.
CASE REPORT
A 32-year male presented to the cardiac emergency unit with complaints of chest pain and shortness of breath, NYHA-3, for 1 day. His baseline echocardiography and CT images were done. It was reported as a case of aortic root and AAA of 6 cm and TBAD (Figure 1). As per the new The Society of Thoracic Surgeons (STS) nomenclature of aortic dissections,5 it was TBAD zone P3 D9. The level of acuity according to the aortic dissection nomenclature was 'high risk’ as the right kidney showed signs of mal-perfusion.
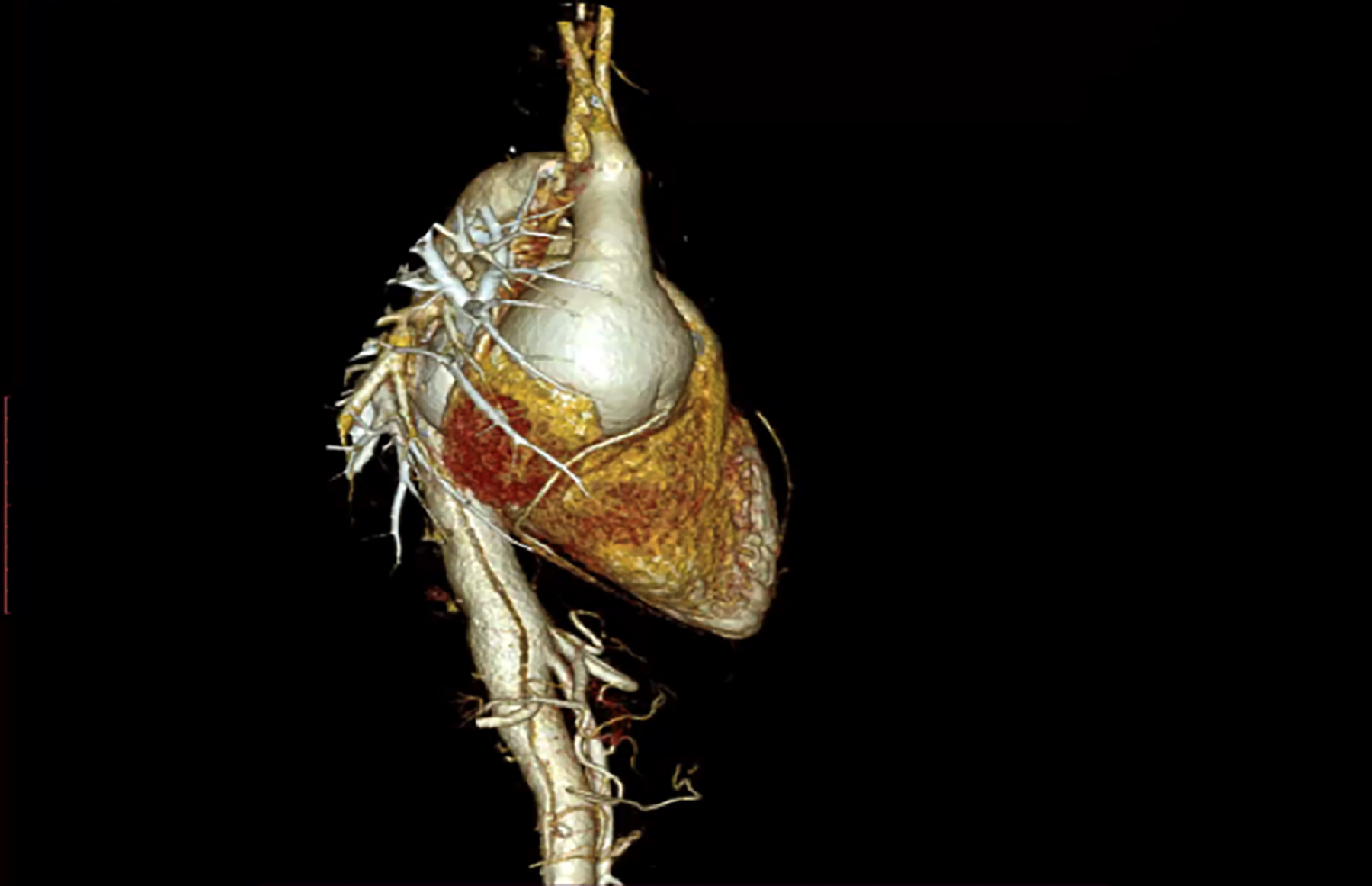 Figure 1: Type B aortic dissection and ascending aorta aneurysm.
Figure 1: Type B aortic dissection and ascending aorta aneurysm.
According to the “New Practice Guidelines Addressing Diagnosis and Treatment of TBAD,”5 optimal medical treatment (OMT) is the class 1 (strong) indication for an uncomplicated TBAD. Prophylactic TEVAR can be considered in patients with an uncomplicated TBAD to reduce the late aortic-related adverse outcomes and aortic-related death – class 2b. Close surveillance after the hospital discharge has been recommended for patients having acute TBAD – Class 1. There are no freely accessible TEVAR facilities in Pakistan and the patient was very poor, so the patient was planned on the following principles: Medical therapy, regular surveillance echocardiograms, and urgent in-hospital operation for aortic root and AAA.
Two days later, the patient had a surveillance echocardiogram that showed a linear echogenic density flap seen in ascending and descending aorta: annulus of 25 mm, sinuses 48 mm, STJ 58 mm, ascending aneurysm 60 mm, arch 24 mm, and descending aorta 25 mm. Additionally, the echocardiogram showed moderate to severe aortic regurgitation (AR), ejection fraction (EF) of 40% and tricuspid annular plane systolic excursion (TAPSE) of 20 mm. So, according to the new nomenclature of STS, it was now Type A D9 aortic dissection. Hence, the following operation was planned “Emergency Type A Aortic dissection repair with aortic root and ascending aorta replacement”.
Right axillary cannulation with an 8 mm Dacron graft was done. Arterial cannula was placed in the artery. Median sternotomy was done and upon incision of pericardium, 300 ml of fresh blood was drained. After suctioning all the blood from the pericardium, a tear on the ascending aorta was visible (Figure 2).
 Figure 2: Tear on ascending aorta.
Figure 2: Tear on ascending aorta.
The pulmonary artery and ascending aorta were completely adherent and very difficult to dissect. The pulmonary artery tore during the dissection that was repaired with the bovine pericardial patch. A transverse aortotomy was done that showed complete dissection of root and ascending aorta. Direct ostial plegia Saint Thomas mixed with cold blood plegia (4:1) was repeated every 20 minutes. Topical ice-cold saline was poured on the heart after every 20 minutes. The proximal end of aorta was done via Modified Bentall procedure and the patient was cooled down to 32 degrees. A 25-sized SJ aortic valve-conduit was used. The distal anastomosis was done on partial circulatory arrest after cooling the patient to 25 degrees, 10 ml/Kg flow was maintained and the patient remained on partial circulatory arrest for 25 minutes. The patient came off the cardiopulmonary bypass smoothly. Hemostasis was secured and the final picture was taken (Figure 3) before closing the sternum.
Figure 3: Final picture after aortic root and ascending aorta replacement.
It was a long operation but the patient did very well. He had a short ICU and ward stay. Initially, he had deranged creatinine and liver function tests but improved later on. He developed hoarseness of voice for which he was referred to ENT. His voice is gradually getting better. His post-operative echo showed a normal functioning aortic valve with an MPG of 7 mmHg, moderate generalised systolic dysfunction with an EF of 35%, and depressed right ventricular (RV) function with TAPSE of 11 mm.
DISCUSSION
It is important to learn the new nomenclature for aortic dissection as it explains the proximal and the distal territory of aortic dissection. Due to the advancement of TEVAR and surgical techniques, such as de-branching, and frozen elephant trunks, it is important to know the extent of the dissection, both proximal and distal. Aggressive medical treatment is the management of choice for an uncomplicated TBAD.6 Ascending aortic aneurysms of more than 6 cm in diameter are at risk of rupture and dissection.7 Therefore, close surveillance of high-risk patients of TBAD, who are currently being treated with OMT, is very important as they may convert to Type A aortic dissection, as happened in this patient. Due to close in-hospital surveillance, conversion of aortic dissection was diagnosed early and managed accordingly.
In conclusion, this case highlights the need for close surveillance in high-risk cases of TBAB for possible development of complications or conversion to Type A aortic dissection, thus necessitating a change in the management approach.
PATIENT’S CONSENT:
Written informed consent was obtained from the patient.
COMPETING INTEREST:
The authors declared no competing interest.
AUTHORS’ CONTRIBUTION:
WS: Contributed to the concept, acquisition of data, and assisted the case as the first assistant.
FAR: Primary surgeon of the case and contributed to the design of research.
FI: Drafting of the manuscript.
All the authors have approved the final version of the manuscript to be published.
REFERENCES
Copyright © 2025. The author(s); published by College of Physicians and Surgeons Pakistan. This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY-NC-ND) 4.0 https://creativecommons.org/licenses/by-nc-nd/4.0/ which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.