

Affiliations
ABSTRACT
We report a rare case of intrauterine molar pregnancy along with ectopic tubal pregnancy. A 33-year woman who had never been pregnant had an ultrasound (US) after 70 days of amenorrhea suggesting partial hydatidiform mole, with a history of ovulation promotion and pathologically confirmed complete hydatidiform mole after uterine suction dilation and curettage. On 4th postoperative day, a US examination before discharge showed an inhomogeneous mass in the left adnexal region with mild lower abdominal pain. On 17th postoperative day, the blood HCG level did not drop as expected and the recheck result still indicated a mass in the left adnexal region, which did not exclude an ectopic hydatidiform mole. A hysteroscopy with a laparoscopic exploration of the left adnexal mass and salpingotomy confirmed a diagnosis of intrauterine hydatidiform mole combined with left tubal pregnancy.
Key Words: Heterotopic pregnancy, Intrauterine hydatidiform mole, Tubal pregnancy.
INTRODUCTION
Heterotopic pregnancy (HP) is an extremely rare pathological pregnancy in which both intrauterine and ectopic pregnancies are present. With the development of assisted reproductive techniques, the incidence of HP has increased from 1 in 30,000 pregnancies to 1 in 3900 pregnancies.1 Hydatidiform mole is a benign gestational trophoblastic disease, and the incidence rates vary by geographic area.2 In Asia, the incidence is about 1 in 500 pregnancies.3 Intrauterine hydatidiform mole combined with ectopic pregnancy is much rarer in clinical practice. High levels of serum HCG lead and atypical clinical symptoms in patients with a hydatidiform mole with ectopic pregnancy should raise the suspicion of this rare concurrence.4
An early diagnosis and appropriate treatment are challenging for these patients. A woman with an intrauterine hydatidiform mole with tubal pregnancy was admitted to our hospital and was successfully managed.
CASE REPORT
A 33-year female was admitted to an outside hospital with a history of amenorrhea for 70 days and a feeling of lower abdominal distention.
This pregnancy was assisted by ovulation-promoting drugs (no exact details). Serum HCG was measured on day 35 of amenorrhea at 24.6 mIU/ml. After that, serum HCG was monitored and gradually increased. On 64th day after amenorrhea, a pelvic ultrasound (US) indicated that "the uterine cavity looks like a gestational sac with no echogenic area". On 70th day after amenorrhea, US was repeated and showed "intrauterine cystic solid echo (size about 5.8×2.8 cm, partial mole?)." The uterus was enlarged to a size of 3-month pregnancy, and the suction evacuation was performed on the same day with ultrasound monitoring. On the second postoperative day, the blood HCG was rechecked at 19,700.7 mIU/ml, and the postoperative pathology reported a complete hydatidiform mole. She was discharged. However, she presented on the fourth postoperative day with mild pain in the left lower abdomen. US showed a heterogeneous echo pattern besides the left ovary. Serum HCG was 4,532 mIU/mL on 17th day postoperatively, and repeat US revealed a mass in the left adnexa (Figure 1 A, B) at our hospital. Considering the non-significant decrease of serum HCG and suspicion of ectopic hydatidiform mole, hysteroscopy combined with laparoscopy was performed. During the operation, about 50 ml of haemoperitoneum was observed in the pelvis. The left fallopian tube thickening of 3×2×2 cm (Figure 1 C, D) was seen laparoscopically. A small amount of decidual-like tissue was scraped from the posterior wall of the uterine cavity by loop electrosurgical excision procedure. A laparoscopic salpingostomy was conducted on the left fallopian tube (Figure 1E). Serum HCG was 974.2 mIU/mL on the first day and 47.5 mIU/mL on the 7th day postoperatively. The postoperative pathological report was consistent with ectopic pregnancy (Figure 1F). The patient recovered well and was discharged for follow-up.
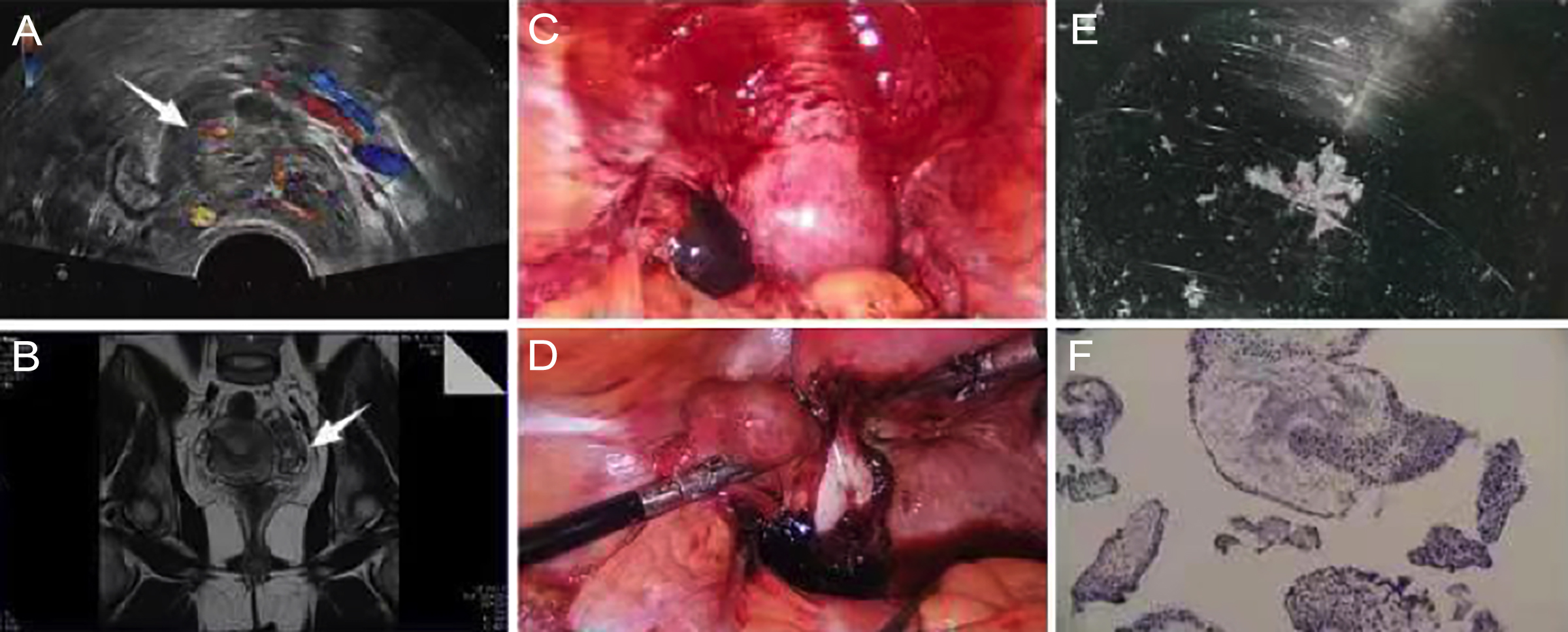 Figure 1: (A) Pelvic ultrasound images (B) Pelvic MRI images (C, D) Peroperative images during laparoscopic exploration (E) Pregnancy tissue in the fallopian tube (F) Histopathological section of left tubal pregnancy (H and E, ×20).
Figure 1: (A) Pelvic ultrasound images (B) Pelvic MRI images (C, D) Peroperative images during laparoscopic exploration (E) Pregnancy tissue in the fallopian tube (F) Histopathological section of left tubal pregnancy (H and E, ×20).
DISCUSSION
We reported an extremely rare case of intrauterine hydatidiform mole with left ectopic tubal pregnancy. HP is a rare natural pregnancy, but with the development of assisted reproductive techniques, the incidence of HP is increasing. The diagnosis of HP is mainly determined by clinical symptoms, signs, the level of serum HCG, US, and laparoscopic exploration. Many patients with HP have no obvious clinical symptoms in the early stage.5 As the gynaecological US had not detected ectopic pregnancy coexisting with intrauterine pregnancy during the initial workup, the diagnosis of HP was missed. Due to intrauterine pregnancy, it is difficult to diagnose ectopic pregnancy by the level of serum HCG.6 When intrauterine hydatidiform mole occurs, the serum level of HCG of such patients is higher than that of normal intrauterine pregnancy, and a high level of serum HCG is more likely to cover up the existence of ectopic pregnancy.7 Therefore, early diagnosis and early treatment of HP are challenging. In this case, the US revealed a mass in the left adnexal region, and the patient had mild abdominal pain on the 4th day postoperatively. But, it was not taken seriously and was the main reason for the missed diagnosis of ectopic pregnancy in this patient. Fortunately, hysteroscopy combined with laparoscopy was performed when the decrease of serum HCG level was not significant after hydatidiform mole removal, which confirmed the final diagnosis, and this patient was treated promptly before rupture. This case reminds us that HP should be considered if the decrease of serum HCG is not significant after hydatidiform mole removal, and US reveals suspicious extrauterine abnormalities. Moreover, in patients with intrauterine hydatidiform mole, if ultrasonography suggests a mass in the adnexal region, it should not be considered as ovarian cyst alone but should be considered as a possible ectopic pregnancy. Further examinations such as pelvic MRI or hysteroscopy are required, and laparoscopic exploration should be performed if necessary. The laparoscopic examination is the gold standard for the diagnosis of HP.8,9 If the decrease of serum HCG level is not significant after hydatidiform mole removal and ultrasound reveal suspicious extrauterine abnormalities, hysteroscopy combined with laparoscopy exploration is recommended as soon as possible to exclude intrauterine residual hydatidiform mole and assist the diagnosis and treatment of HP.
In conclusion, this case highlights the need to consider the possibility of HP in case of persistent HCG elevation and atypical clinical and ultrasonographic features in women of childbearing age.
PATIENT’S CONSENT:
Informed consent has been obtained from the patient to publish the case.
COMPETING INTEREST:
The authors declared no financial or other relationships that might lead to a competing interest related to this study.
AUTHORS’ CONTRIBUTION:
WJ: Contributed to the conception of the study.
WR: Performed the experiment and wrote the manuscript.
ZY: Contributed significantly to analysis and manuscript preparation.
LJ: Performed the data analyses.
LY: Helped perform the analysis with constructive discussions.
All the authors have approved the final version of the manuscript to be published.
REFERENCES