

Affiliations
ABSTRACT
Trichobezoar is a rare and potentially dangerous surgical condition in which patients swallow their own hair, often as a result of trichotillomania or trichophagia. This case report focuses on a 12-year female who experienced abdominal pain, anaemia, and gastric perforation due to her mental health conditions. Further examination revealed the presence of hairs, fibers, and bile in her stomach wall - indicative of trichobezoar - which had to be surgically removed. It is important for paediatric surgeons to remain aware and informed about this condition so that prompt treatment can be provided when necessary. The patient in this case was also treated with therapy for underlying mental health issues. With careful diagnosis and treatment plans tailored to each individual's needs, patients suffering from trichobezoar can receive the help they need for successful recovery.
Key Words: Bezoars, Gastric rupture, Trichotillomania, Emotional disturbance.
INTRODUCTION
Trichobezoar is a rare medical condition where hairs that have been swallowed accumulate in the stomach or intestines, potentially leading to serious complications such as obstruction, ulcers, bleeding, and even perforation in the digestive tract.1 Trichotillomania is a mental disorder in which people feel compelled to pull out and eat their own hair, even though they may deny the behaviour when asked. It is an impulse control disorder that affects around 2% of the population. People often have tension before pulling out their hair, but experience satisfaction afterwards.2
This case reports a 12-year female with a rare condition called Trichobezoar with gastric perforation. This can be linked to psychological disorders, such as depression and anxiety, which may increase the risk of intestinal perforation and pneumoperitoneum. This is an extraordinary situation and clinicians should be aware of the possible causes, complications, and treatments.
CASE REPORT
A 12-year female presented to the emergency department with abdominal pain, constipation, and distension. On examination, the patient had abdominal tenderness, an elevated temperature of 101˚F, a rapid heart rate of 120 beats per minute, and low blood pressure measuring 90/60 mmHg.
The X-ray revealed the presence of gas throughout the patient's abdomen, which was also seen overlapping the liver (Figure 1). Resuscitative measures were taken upon arrival at the hospital. A review of the family history revealed that the patient was an adopted child, raised by a single mother, who noticed that at the age of two, patches of her hair began to be missing due to her sucking on her head hairs. The results of the laboratory tests indicated that the patient was only suffering from iron deficiency anaemia, i.e., microcytic, hypochromic red blood cells with a haemoglobin of 9.5 g/dl.
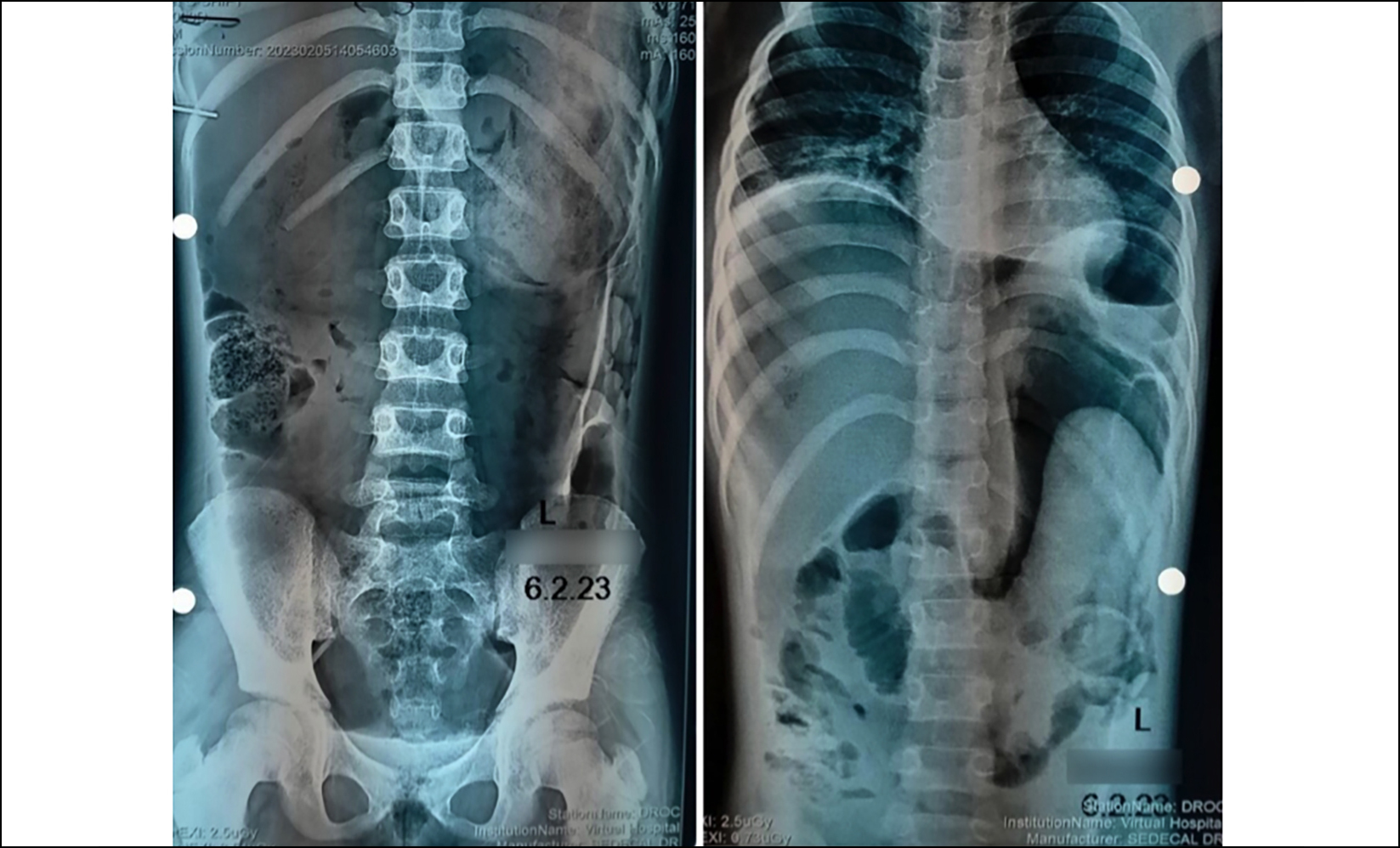 Figure 1: Free air in the abdomen secondary to gastric perforation.
Figure 1: Free air in the abdomen secondary to gastric perforation.
Exploration revealed a 2 × 2 cm perforation in the anterior wall of the stomach. Upon further inspection, this opening revealed a large mass composed of hair, fibrous materials, and bile debris extending from the fundus to the pylorus. This accumulation of material caused significant distension within the stomach and ultimately led to its perforation (Figure 2). To remove the mass, the perforation size was increased and the opening of the stomach that resulted from this procedure was repaired with absorbable sutures in a single layer. After the procedure was completed, the patient made a successful recovery and underwent psychological therapy to confront the underlying issue of trichotillomania with trichophagia which had yet to be identified before gastric perforation. Further evidence for this diagnosis included a scarred area of alopecia (Figure 3).
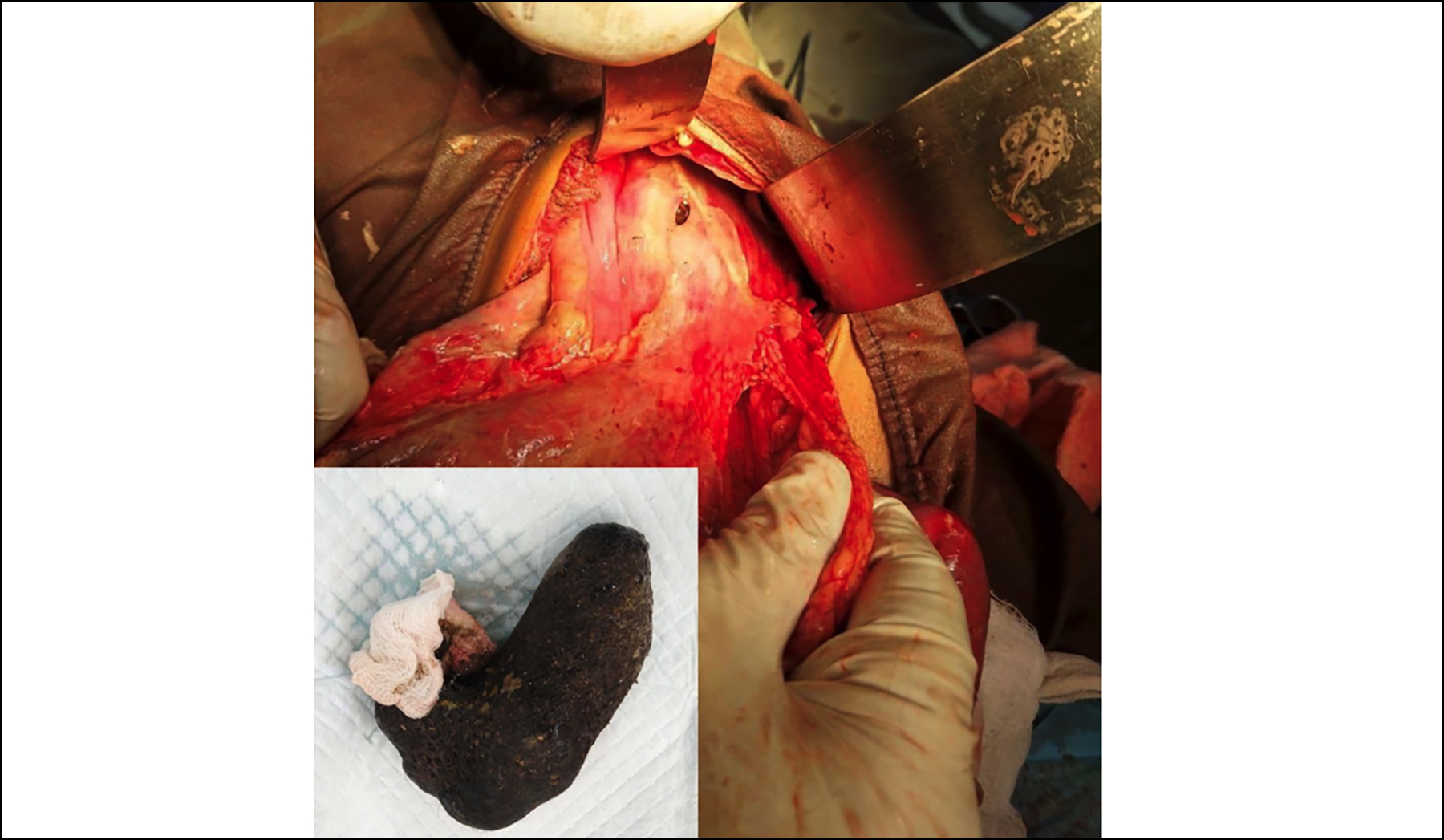 Figure 2: Surgical removal of trichobezoar mass (inset) through a single perforation on the anterior surface of the stomach.
Figure 2: Surgical removal of trichobezoar mass (inset) through a single perforation on the anterior surface of the stomach.
 Figure 3: A scarred area of alopecia on the patient’s head.
Figure 3: A scarred area of alopecia on the patient’s head.
DISCUSSION
Bezoar is a term used to describe an accumulation of foreign material which can be found in both the stomach and small intestine. These masses, known as bezoars, are categorized in three types; trichobezoars are composed of hair, phytobezoars consist of indigestible plant fiber matter, and trichophytobezoars combine these two components – hair and vegetable/fruit fibers.3 Trichobezoars can cause several complications, including gastric ulcers (10% of cases), intestinal obstruction (up to 11%), and the perforation of the digestive tract. In some instances, a piece of the hairball may detach from the stomach leading to perforation of the ileum.4 This patient presented with peritonitis, and initially a psychological disorder or trichobezoar was not considered as the primary diagnosis. However, upon surgery, it was confirmed that the patient had been eating her own hair. This is an incredibly rare complication, with only a few cases reported in the literature. Mechanical irritation of the gastric mucosa and obstruction of the pyloric ring by a trichobezoar could lead to increased acid secretion, gastric ulceration, and potentially life-threatening complications such as gastric perforation.5-7
In conclusion, Trichobezoars can be extremely dangerous due to their potential to cause gastric ulcers, intestinal obstruction, and perforation. It is important for medical professionals to remain aware of this rare complication as it can have serious consequences if not treated promptly.
PATIENT’S CONSENT:
Written informed consent was obtained from the patient’s family to publish this case.
COMPETING INTEREST:
The authors declared no competing interest.
AUTHORS’ CONTRIBUTION:
IAQ, MAQ: Conception of study, manuscript writing, and critical review.
AHZ, IA, MH: Facilitation and material provision.
All the authors have approved the final version of the manuscript to be published.
REFERENCES